
Exercise for Your Feet
Foot and ankle pain can be a nuisance in a person’s life, especially if it happens frequently. The best way to prevent this type of pain, is to exercise often. Regular exercise of the foot includes stretching and strength exercises. Stretching exercises can help prevent injuries such as a sprained ankle, while strength exercises can prevent ailments such as plantar fasciitis.
Stretching exercises can help improve flexibility and the foot and ankle’s range of motion. These exercises can certainly help with those who participate in high-energy activities such as sports. Many athletes routinely perform foot and ankle exercises to prevent injuries like sprained ankles, which are common injuries where the tendons in the ankle are over stretched. Strength exercises help develop foot muscles for better support and protection.
Most exercises are simple and can be done at home, either standing or sitting. One chair exercise is called “limber up”. In this exercise, a person would start by sitting down with their feet flat on the floor. Then lift one leg up so the feet are not touching the floor, then rotate your foot clockwise 15-20 times, and 15-20 times counterclockwise. Repeat the same process with the opposite leg. Another sitting exercise helps stretch the back of your heel and requires an exercise band. It begins by looping the band around a heavy piece of furniture, or something stable that will not be moved when the band is tugged or pulled. Then sit directly in front of it, and slide one foot into the loop, so that the band curves around the forefoot. Start by pulling the forefoot back and holding it for 5-10 seconds. Doing this 10-15 times on each foot, will stretch the back of your heel, increasing your flexibility.
Foot exercises that require standing are also just as easy and simple. Referred as the “Achilles Stretch”, this exercise stretches the Achilles tendon, making it more flexible, helping prevent foot, ankle, and leg pain. It begins by first standing and facing the wall, with the arms outstretched and the palms on the wall. Then place one foot behind another keeping the back leg straight, and the forward leg bending at the knee. Make sure both heels are flat on the floor and adjust your stance accordingly. With your hips, lean forward to feel the stretch, you can also adjust the distance from your feet to feel the stretch in various parts of the calf. Make sure to hold the stretch for about 30 seconds and repeat the same process 3 times with each leg. An even easier foot exercise is simply walking on sand. Walking barefoot on sand both strengthens and stretches your feet.
Doing these exercises regularly can help prevent many foot and ankle problems. Other foot exercises can even relieve pain. For example, those affected with plantar fasciitis can simply sit down on a chair, and then place a tennis ball below their affected foot. By rolling the ball under the foot, and increasing or decreasing pressure, pain will be relieved. With any exercise, it is always important to do a small warmup such as walking a few laps around the house to get the blood flowing. If after doing an exercise to relieve pain such as the tennis ball exercise, or are unsure that your execution is correct, be sure to contact a podiatrist for further instruction.
Treating Heel Pain With Extracorporeal Shockwave Therapy
Extracorporeal Shockwave Therapy (ESWT) is an FDA-approved treatment for plantar fasciitis, the most common form of heel pain. ESWT delivers targeted high-energy sound waves to the injured and inflamed plantar fascia tissue. This process breaks up scar tissue and encourages the body to create new tissue cells which, in turn, stimulates healing and reduces pain. Acoustic wave therapy has been used for decades in shockwave lithotripsy—a treatment that breaks up kidney stones. ESWT is safe, non-invasive, and treatments generally take less than half an hour on each foot, with typically 3-5 sessions needed for many patients to begin to feel relief. If you have plantar fasciitis, contact a podiatrist to discuss whether you may be a good candidate for ESWT.
Shockwave therapy is a treatment commonly used to treat various injuries and conditions, particularly plantar fasciitis in the feet. To learn more, consult with Dr. Randy Garr from Bigfoot Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Shockwave Therapy
Shockwave therapy is a new treatment option designed to treat bone conditions such as tennis elbow, shoulder pain, and others. Shockwave therapy uses high intensity sound waves that are directed to the affected tissues of the body with pinpoint accuracy. The effects are very beneficial, leading to a production of collagen fibers, eliminating inflammation.
Who Benefits from Shockwave?
Shockwave is recommended for patients suffering from heel pain and associated problems. Heel pain is a common condition which can be caused by obesity, overexertion, and spending a substantial amount of time on hard floors with your feet exposed and unsupported.
Fast and Easy
The therapy is actually a simple process that can leave patients feeling better the very next day. Shockwave therapy is not as dramatic as it sounds. It enables more blood flow to effected areas, addressing the source of the problem and allowing treatment to last for a long time.
Treatment & Recovery Time
Shockwave treatment will enable your feet to recover quickly. This is especially important since surgery is not required. It is cost effective and does not require the use of anesthesia. This treatment is a better option to surgery, since it is proven safe.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Heel Pain with Shockwave Therapy
Shockwave therapy is one treatment option for plantar fasciitis, a condition that causes heel and foot inflammation and pain. This type of injury is often caused by overworking the feet. Heel pain is most common in people that exercise often, individuals who are overweight, and people whose profession require them to stand for long periods of time.
Heel pain can be caused by a number of problems including ill-fitting shoes, strenuous exercise routines or work hazards. Simple treatment options involve buying new shoes, taking ibuprofen, doing heel and foot exercises, and resting your feet. For severe cases, shockwave therapy can be considered a more viable form of treatment.
Shockwave therapy should be considered for patients that have had unsuccessful treatment or whose heel pain has lasted for more than six months. In shockwave therapy, a device delivers shockwaves to the patient’s body, which jumpstart the body’s repair mechanisms. These mechanisms then begin working more effectively to repair damage done to the heel area.
Shockwave therapy also helps eliminate pain in the heel area. When the body’s natural repair mechanisms are triggered, tissue healing in the body is sped up. This leads to pain reduction after pain transmission nerves are stimulated.
Shockwave therapy eliminates the risk factors associated with surgery, such as the use of anesthetics, and is less invasive. Since this technique also helps improve the body’s natural healing techniques, recovery time should be shorter than surgical procedures.
Discomfort issues can also be a side effect of treatment. Short-term issues normally include skin bruising, minor pain during and after treatment, swelling of the heel, and discolored tissue. However, these side effects of shockwave therapy usually disappear after a few days. The fast recovery time of shockwave therapy makes it easy for patients to return to their daily routines.
Like most types of treatments, surgeries, and medications, shockwave therapy is not for everyone. Potential patients with heart conditions and people with pacemakers should not be considered for this technique. People on certain types of medications, usually medications affecting blood clotting, would be ineligible for shockwave therapy. Children and pregnant women should avoid this treatment option as well.
Overall, shockwave therapy could be a great option for heel pain. It is less invasive than surgery, helps trigger natural healing mechanisms, and should be considered by people who have had long bouts of heel pain or tried conventional treatment options that were unsuccessful.
Key Differences Between Store-Bought and Custom Orthotics
 While at first glance, you may assume that there is no difference between over-the-counter (OTC) insoles and custom orthotics, a closer look reveals several key distinctions. OTC insoles are a “one-size-fits-most,” generic approach to supporting your feet. Custom orthotics are customized, prescription medical devices. Your podiatrist starts by reviewing your medical history, examining your feet and diagnosing your condition. Custom orthotics are then created from molds or 3D images of your actual feet. They are designed to specifically treat your medical condition: from arthritis, flat feet and hammertoes to bunions, high arches, deformities, plantar fasciitis and more. Custom orthotics can also help correct certain gait abnormalities and restore function in your feet and ankles. OTC, or prefabricated insoles, are typically made of rubber, flexible plastic or gel which can often lose integrity quickly. Custom orthotics are constructed with superior materials that are durable, light weight, moldable, and cushioning. If you are suffering from foot or ankle pain, or have difficulty walking, see a podiatrist. They will evaluate and diagnose your condition and discuss if custom orthotics can provide the relief you seek.
While at first glance, you may assume that there is no difference between over-the-counter (OTC) insoles and custom orthotics, a closer look reveals several key distinctions. OTC insoles are a “one-size-fits-most,” generic approach to supporting your feet. Custom orthotics are customized, prescription medical devices. Your podiatrist starts by reviewing your medical history, examining your feet and diagnosing your condition. Custom orthotics are then created from molds or 3D images of your actual feet. They are designed to specifically treat your medical condition: from arthritis, flat feet and hammertoes to bunions, high arches, deformities, plantar fasciitis and more. Custom orthotics can also help correct certain gait abnormalities and restore function in your feet and ankles. OTC, or prefabricated insoles, are typically made of rubber, flexible plastic or gel which can often lose integrity quickly. Custom orthotics are constructed with superior materials that are durable, light weight, moldable, and cushioning. If you are suffering from foot or ankle pain, or have difficulty walking, see a podiatrist. They will evaluate and diagnose your condition and discuss if custom orthotics can provide the relief you seek.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Randy Garr from Bigfoot Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
What Is Wound Debridement?
 A diabetic foot ulcer (DFU) is a type of wound that can develop on the lower limbs of people with diabetes. These wounds typically heal slowly and poorly and are at an increased risk of becoming infected. Sometimes debridement is necessary to treat a DFU. Debridement is the process of removing dead or damaged skin, tissue, and debris from a wound to help it heal. During debridement, the podiatrist will clean and disinfect the wound, then probe it with a metal instrument to check how deep the wound is and if there are any foreign objects in it. The podiatrist will then cut away dead tissues and wash out the DFU. This is generally done under local or general anesthesia. Not all debridement involves cutting away dead tissues. Depending on the needs of the patient, it may also be possible to debride the wound with special enzymes, dressings, and more. If you have DFUs, it is suggested that you are under the care of a podiatrist.
A diabetic foot ulcer (DFU) is a type of wound that can develop on the lower limbs of people with diabetes. These wounds typically heal slowly and poorly and are at an increased risk of becoming infected. Sometimes debridement is necessary to treat a DFU. Debridement is the process of removing dead or damaged skin, tissue, and debris from a wound to help it heal. During debridement, the podiatrist will clean and disinfect the wound, then probe it with a metal instrument to check how deep the wound is and if there are any foreign objects in it. The podiatrist will then cut away dead tissues and wash out the DFU. This is generally done under local or general anesthesia. Not all debridement involves cutting away dead tissues. Depending on the needs of the patient, it may also be possible to debride the wound with special enzymes, dressings, and more. If you have DFUs, it is suggested that you are under the care of a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Randy Garr from Bigfoot Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Tarsal Tunnel Syndrome and Rheumatoid Arthritis
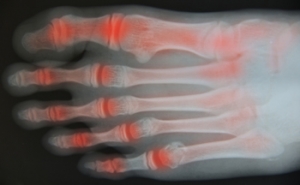
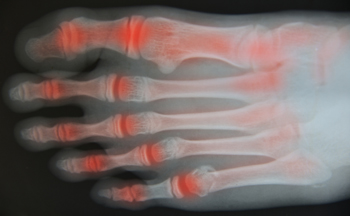 Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.